Incision and drainage (I&D) of a buccal space infection is a surgical procedure to treat an abscess located between the buccinator muscle and the overlying skin of the cheek. It’s important to understand the anatomy and maintain sterile technique. This is typically performed by oral and maxillofacial surgeons or trained physicians.
Here’s a step-by-step overview of the procedure:
1. Preoperative Preparation
-
Clinical assessment: Confirm buccal space involvement via clinical signs (swelling of the cheek, pain, erythema) and possibly imaging (CT scan or ultrasound).
-
Medical optimization: Address underlying conditions (e.g., diabetes).
-
Informed consent: Discuss risks like nerve injury, scarring, recurrence, or fistula formation.
-
Antibiotics: Start empiric IV antibiotics targeting oral flora (e.g., ampicillin-sulbactam, or clindamycin if allergic).
2. Anesthesia
-
Local anesthesia: Lidocaine with epinephrine is infiltrated in the area.
-
Sedation or general anesthesia may be needed for uncooperative or pediatric patients.
3. Incision Technique
-
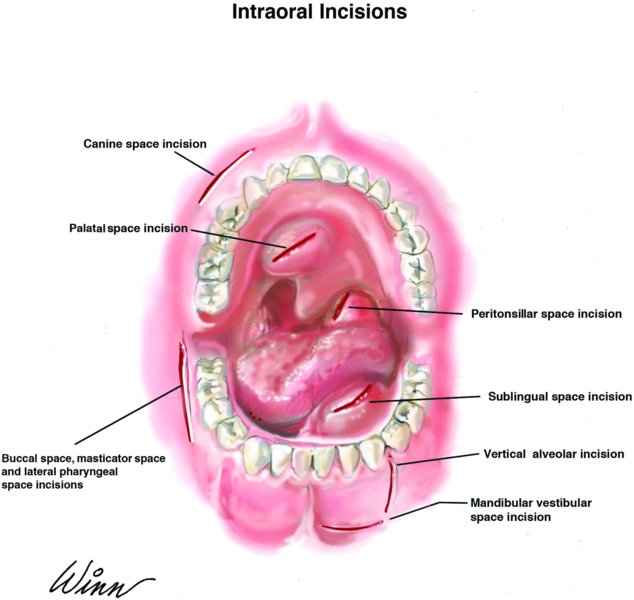
Intraoral approach (preferred if accessible):
-
Make a 1.5–2 cm incision in the mucosa, typically in the maxillary vestibule near the molars, avoiding the parotid (Stensen’s) duct.
-
Blunt dissection with a hemostat to reach and break up the abscess cavity.
-
-
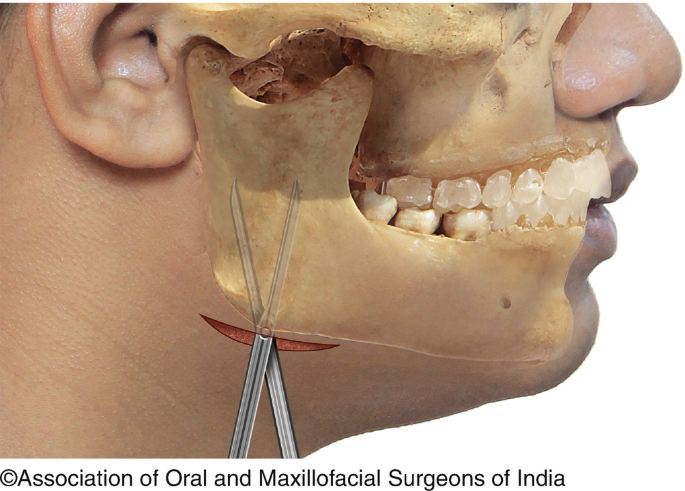
Extraoral approach (if intraoral access is not feasible):
-
Make a 2–3 cm incision about 1.5 cm below and lateral to the oral commissure, parallel to natural skin creases (cosmetic consideration).
-
Blunt dissection through subcutaneous tissue to reach the abscess cavity, taking care to avoid the facial nerve branches and parotid duct.
-
4. Drainage and Irrigation
-
Express purulent material; culture the pus.
-
Irrigate the cavity thoroughly with sterile saline.
-
Break up loculations using a hemostat.
5. Drain Placement
-
Place a Penrose drain or corrugated drain to allow continuous drainage.
-
Secure the drain with a suture.
-
For intraoral incisions, passive drainage may be sufficient depending on the cavity.
6. Postoperative Care
-
Continue antibiotics.
-
Warm compresses to the area.
-
Drain care and regular follow-up.
-
Remove the drain in 2–5 days when drainage subsides and infection resolves.
Important Considerations
-
Avoid vital structures (facial artery, vein, nerve).
-
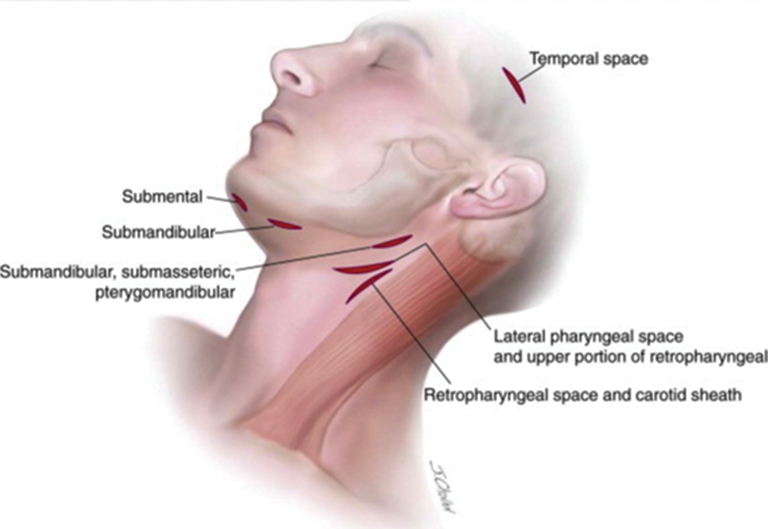
Differentiate buccal space from deeper infections (e.g., masticator or parapharyngeal).
-
Consider hospitalization for systemic signs or deep space involvement.