Paradoxical worsening of truncal acne with doxycycline refers to a situation where the use of doxycycline, a commonly prescribed antibiotic for treating acne, leads to a temporary or unexpected worsening of acne, particularly on the trunk (chest, back, etc.).
Though rare, this paradoxical effect can occur due to several possible reasons:
-
Overgrowth of resistant bacteria: Doxycycline works by targeting Propionibacterium acnes, a bacterium involved in acne. However, over time, some strains of bacteria may become resistant to the antibiotic. The overgrowth of resistant bacteria can cause an exacerbation of acne.
-
Immune system reaction: Doxycycline, being an antibiotic, may trigger an inflammatory response or hypersensitivity reaction in some people. This could lead to an increase in acne lesions as part of the body’s response to the drug.
-
Changes in skin microbiome: Antibiotics, including doxycycline, can alter the skin’s natural microbiome. This disruption might lead to the overgrowth of other microorganisms that could worsen acne, especially on the trunk.
-
Hormonal fluctuations: Acne on the trunk may be more strongly influenced by hormonal changes, and in some cases, doxycycline could indirectly affect hormonal levels or interactions, leading to a flare-up.
-
Incorrect use or dosage: Sometimes, using doxycycline incorrectly (e.g., taking it inappropriately or for an incorrect duration) might lead to an imbalance that worsens the condition.
How to Manage Paradoxical Worsening:
If you’re experiencing this paradoxical worsening while on doxycycline, it’s important to:
- Consult your healthcare provider: A dermatologist may recommend switching to a different antibiotic or acne treatment.
- Adjust the dosage: Sometimes, reducing the dosage can help minimize side effects.
- Combination therapy: Using doxycycline alongside topical treatments, such as benzoyl peroxide, retinoids, or other medications, may help prevent acne from worsening.
- Monitor the skin’s response: Keeping track of how your skin is responding to the treatment can help your doctor make more informed decisions.
Mechanisms Behind Paradoxical Worsening
-
Antibiotic Resistance:
- Bacterial Resistance: One of the most well-documented causes of paradoxical worsening is the development of resistance in Propionibacterium acnes (now renamed Cutibacterium acnes). Prolonged or inappropriate use of doxycycline can encourage the development of resistant strains of C. acnes, which may proliferate and cause increased inflammation, leading to worsening of acne.
- Reference:
- “Antibiotic resistance in acne treatment: A review of the current evidence” (Journal of Clinical and Aesthetic Dermatology, 2015). This paper reviews the role of antibiotic resistance in acne management, particularly in relation to C. acnes.
- “Antibiotic resistance in acne: A cause for concern?” (Journal of Drugs in Dermatology, 2011) discusses the increasing problem of antibiotic resistance and its impact on acne treatment.
-
Alteration of the Skin Microbiome:
- Disruption of Normal Flora: Antibiotics like doxycycline may disrupt the normal skin microbiome, which includes beneficial bacteria that help keep acne-causing bacteria in check. With the reduction in beneficial bacteria, there may be an overgrowth of other microorganisms, which could exacerbate acne.
- Reference:
- “The human skin microbiome: A possible link to acne vulgaris?” (Journal of Investigative Dermatology, 2017). This article discusses how the microbiome influences skin conditions like acne and how antibiotics may alter this balance.
- “The role of the skin microbiome in the pathogenesis of acne vulgaris” (Journal of Dermatological Science, 2020) explains how changes to the skin microbiome could result in worsened acne or even paradoxical flare-ups.
-
Immune Response or Hypersensitivity:
- Inflammatory Reaction: Doxycycline is known to have some anti-inflammatory effects, but paradoxically, it can also trigger inflammatory or hypersensitivity reactions in certain patients. These reactions may not be immediately obvious and could manifest as worsening acne.
- Reference:
- “Cutaneous reactions to antibiotics: Review and update” (American Journal of Clinical Dermatology, 2016). This review addresses hypersensitivity reactions and other side effects that can occur with antibiotics like doxycycline.
- “Antibiotic-induced hypersensitivity reactions” (Dermatology Research and Practice, 2012) discusses the potential for doxycycline to cause inflammatory or allergic responses in some individuals.
-
Hormonal Fluctuations:
- Hormonal Changes: Acne, particularly on the trunk, is often hormonally driven. Doxycycline itself may not directly affect hormones, but its antibiotic action could lead to subtle changes in hormone regulation. For example, the disruption of the gut microbiome could potentially affect hormone metabolism and exacerbate acne.
- Reference:
- “The role of hormones in acne vulgaris” (Dermatology Research and Practice, 2012) explores the link between hormonal changes and acne development, highlighting how fluctuations can lead to worsened skin conditions.
- “Gut microbiome and its impact on hormonal regulation” (Journal of Endocrinology, 2019) discusses how the gut microbiome (which doxycycline affects) might influence hormones.
-
Incorrect Use or Dosage:
- Overuse or Inconsistent Dosing: Using doxycycline for extended periods without proper management or for conditions where it isn’t fully effective could lead to paradoxical reactions. Acne might worsen due to an improper dosing schedule or use beyond the recommended duration.
- Reference:
- “Doxycycline in acne vulgaris: A review of the literature” (Clinical, Cosmetic and Investigational Dermatology, 2016). This article provides an overview of the effectiveness and appropriate use of doxycycline in acne treatment, including potential side effects and misuse.
Clinical Evidence and Case Reports
Several case reports and studies have discussed paradoxical worsening of acne with doxycycline use:
-
“Paradoxical acne exacerbation associated with oral antibiotics” (Journal of Clinical and Aesthetic Dermatology, 2010): This article provides case studies where patients experienced an increase in acne symptoms after starting antibiotics like doxycycline. In some cases, the worsening was linked to antibiotic resistance or changes in the skin microbiome.
-
“Acne exacerbation with doxycycline: An unexpected side effect” (Dermatology Times, 2012): This case series reports on patients whose acne worsened with the use of doxycycline, highlighting the need for careful monitoring when prescribing antibiotics for acne.
Management of Paradoxical Worsening
If you experience paradoxical worsening of acne while on doxycycline, management strategies include:
-
Reevaluation of the treatment: Discontinuing doxycycline or switching to a different antibiotic, such as minocycline or tetracycline, may be considered. Sometimes, topical treatments like retinoids or benzoyl peroxide are recommended instead of systemic antibiotics.
-
Adjunctive therapies: Dermatologists may recommend the use of topical antibiotics, retinoids, or hormonal treatments (like oral contraceptives or anti-androgens) to address both the acne and the inflammatory response caused by doxycycline.
-
Probiotics: Since doxycycline can disrupt the skin’s microbiome, some studies suggest that using probiotics may help restore balance, though the evidence is still developing.
-
Reducing duration: Shortening the duration of doxycycline use or employing pulse therapy (intermittent treatment) can help reduce the risk of paradoxical worsening.
Conclusion
While doxycycline is widely used to treat acne, its paradoxical worsening, particularly on the trunk, is likely a result of antibiotic resistance, disruption of the skin microbiome, immune responses, or hormonal fluctuations. If this occurs, working closely with a healthcare provider to adjust treatment is essential. Reviewing the available literature and understanding the mechanisms behind this paradox can help manage and prevent such compli
cations.
References:
- “Antibiotic resistance in acne treatment: A review of the current evidence” (Journal of Clinical and Aesthetic Dermatology, 2015).
- “Antibiotic-induced hypersensitivity reactions” (Dermatology Research and Practice, 2012).
- “Paradoxical acne exacerbation associated with oral antibiotics” (Journal of Clinical and Aesthetic Dermatology, 2010).


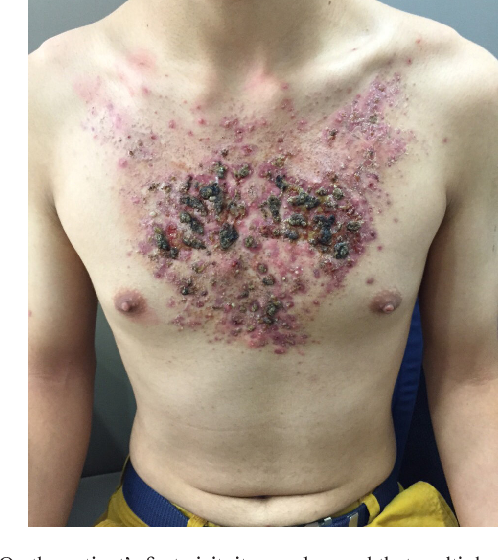
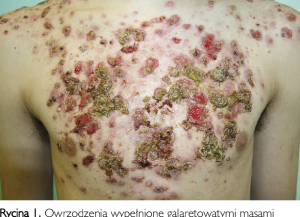
Chest of a male patient with acne fulminans. This is a rare severe form of acne where there are ulcerative lesions on the skin as well as systemic symptoms such as fever and joint pain. It is thought to be caused by an immune response to increased testosterone levels and the presence of Cutibacterium acnes bacteria.