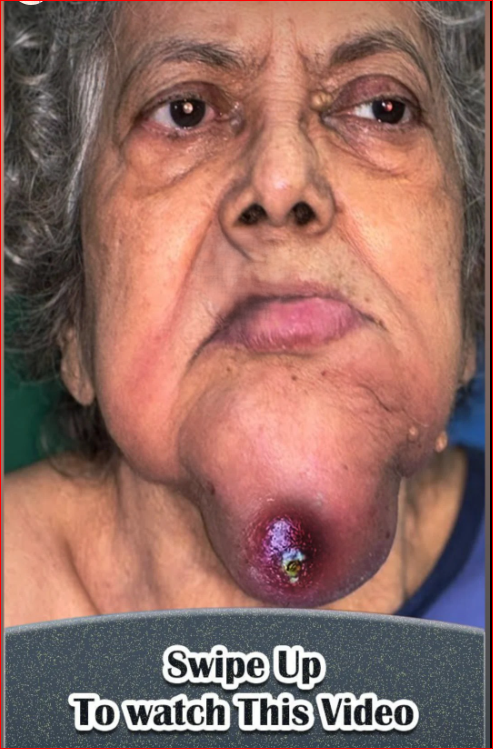
A large metastatic node refers to a lymph node that has grown in size due to the spread of cancer cells from a primary tumor to the lymphatic system. These nodes are commonly referred to as “lymph node metastasis” and can be found in various parts of the body, depending on where the cancer originated. The size and extent of the node enlargement often indicate the stage of cancer progression.
The management or evaluation of a large metastatic lymph node typically involves several steps:
1. Diagnosis:
- Imaging: To assess the size and characteristics of the lymph node(s), various imaging techniques are used, including:
- CT (Computed Tomography) Scan
- MRI (Magnetic Resonance Imaging)
- Ultrasound: Helps to identify the size and structure of the node.
- PET (Positron Emission Tomography) Scan: Can show areas of high metabolic activity, which often correlates with cancer.
- Biopsy: The most definitive way to diagnose a metastatic node is through biopsy, where a sample of tissue from the lymph node is examined under a microscope. This can be done via:
- Fine Needle Aspiration (FNA): A small needle is used to extract cells from the lymph node.
- Core Needle Biopsy: A larger needle is used to remove a small cylinder of tissue.
- Excisional Biopsy: The entire lymph node is removed surgically for examination.
2. Staging: The stage of cancer is crucial for determining the treatment plan and prognosis. The size of the metastatic lymph node plays a role in staging:
- Stage I/II: Early-stage cancers with smaller nodes.
- Stage III/IV: Later stages with larger, multiple nodes involved, indicating more advanced disease.
3. Treatment:
The treatment for large metastatic nodes depends on several factors, including the type and location of the cancer, as well as the overall health of the patient. Treatment options include:
- Surgery: If the metastatic node is localized and accessible, surgery may be used to remove it. However, removal of large or multiple nodes may not always be possible.
- Radiation Therapy: Used to target metastatic nodes, especially when they are in areas that are difficult to operate on.
- Chemotherapy: If the cancer has spread more widely, chemotherapy might be used to treat both the primary tumor and the metastatic nodes.
- Targeted Therapy/Immunotherapy: Some cancers can be treated with drugs that target specific mutations or boost the body’s immune system to fight cancer.
4. Follow-Up:
After treatment, follow-up imaging and monitoring are important to ensure that the metastatic nodes do not grow again or that new ones do not develop.
Factors that Affect the Size of the Node:
- Tumor Biology: The type of cancer (e.g., melanoma, breast cancer, lung cancer) and how aggressive it is can influence the size of metastatic nodes.
- Time of Detection: The longer a metastatic node has been present, the larger it might grow.
- Treatment Response: Some treatments, such as chemotherapy or radiation, may shrink the size of metastatic nodes.
1. Diagnosis of Large Metastatic Nodes
The diagnosis of metastatic lymphadenopathy is multi-step and typically involves the following:
a. Imaging Techniques:
-
CT Scans: The most commonly used imaging modality for evaluating the size and characteristics of metastatic lymph nodes. A CT scan can show enlarged lymph nodes and provide a clearer understanding of their location and proximity to other organs or structures. According to the American College of Radiology (ACR), CT imaging is a standard for detecting lymph node metastasis, with specific criteria used to measure node size (nodes > 1 cm in short-axis are considered suspicious for metastasis) (ACR Appropriateness Criteria).
-
MRI: Useful for assessing deep lymph nodes, particularly those near critical structures such as the central nervous system or abdominal organs. MRI is especially valuable when there are concerns about soft tissue infiltration or neurological involvement (e.g., J Natl Cancer Inst Monogr, 2012).
-
Ultrasound: High-resolution ultrasound can detect lymph node enlargement, and it’s often used for superficial nodes. The British Journal of Radiology (2015) notes ultrasound is a cost-effective method for initial screening, with the ability to guide biopsies.
-
PET Scan: A Positron Emission Tomography scan is very useful in assessing metabolic activity within lymph nodes. It highlights areas with abnormal glucose metabolism, which can correspond to tumor cells. This is often used in conjunction with CT scans in a PET/CT fusion scan to better localize and stage the cancer (Journal of Clinical Oncology, 2006).
b. Biopsy Techniques:
-
Fine Needle Aspiration (FNA): FNA is one of the least invasive methods for diagnosing metastatic lymphadenopathy. However, its sensitivity can be limited by the quality of the sample obtained, and its accuracy can vary depending on the size of the node and the experience of the practitioner (Cytopathology, 2008).
-
Core Needle Biopsy: This method involves extracting a larger tissue sample and provides better diagnostic yield, especially for larger nodes. Studies such as one in the Annals of Surgical Oncology (2005) showed core needle biopsies to be more accurate than FNA, particularly for larger nodes.
-
Excisional Biopsy: If less invasive methods do not provide sufficient diagnostic clarity, excisional biopsy (removal of the entire lymph node) may be considered. This is often necessary when nodes are large or when there is concern for a high-grade tumor (Cancer Research UK, 2019).
2. Staging and Prognostic Implications
The presence of large metastatic lymph nodes affects cancer staging, which influences treatment decisions. In The AJCC Cancer Staging Manual (8th Edition), lymph node involvement is categorized as follows:
- N0: No regional lymph node metastasis.
- N1: Metastasis in 1–3 regional lymph nodes.
- N2: Metastasis in 4–9 regional lymph nodes.
- N3: Metastasis in 10 or more regional lymph nodes.
For example, in breast cancer, involvement of large lymph nodes (e.g., nodes > 2 cm) is considered indicative of more advanced disease and often corresponds to higher-grade tumors (JAMA, 2014).
3. Treatment of Large Metastatic Nodes
Treatment strategies for metastatic nodes depend on the underlying cancer, but generally involve a combination of surgery, chemotherapy, radiation therapy, and sometimes newer immunotherapy/targeted therapies.
a. Surgical Management:
- Lymph Node Dissection: In certain cancers, such as melanoma or breast cancer, surgery to remove affected lymph nodes can be both diagnostic and therapeutic. Sentinel lymph node biopsy (SLNB) is commonly used to detect early-stage metastasis and guide decisions about further dissection. For example, in early-stage melanoma, the removal of the sentinel lymph node may reduce the risk of further metastasis (Lancet Oncology, 2004).
b. Chemotherapy:
- Chemotherapy is used when lymph node involvement is part of more widespread disease, particularly in cancers like breast cancer, non-small cell lung cancer (NSCLC), and colorectal cancer. Chemotherapy is often used before surgery (neoadjuvant) or after surgery (adjuvant) to shrink tumors or reduce the risk of recurrence (Cancer Chemotherapy and Pharmacology, 2008).
c. Radiation Therapy:
- For patients with large metastatic nodes that cannot be removed surgically, radiation therapy is often used to target the affected nodes. The use of radiation has been extensively studied, with evidence from Radiotherapy and Oncology (2017) showing its efficacy in controlling enlarged metastatic nodes in cancers such as head and neck cancer, breast cancer, and lymphoma.
d. Targeted Therapy and Immunotherapy:
-
Advances in cancer treatment have led to the development of targeted therapies and immunotherapies. For instance, immune checkpoint inhibitors such as pembrolizumab and nivolumab have shown significant promise in treating cancers like melanoma and non-small cell lung cancer with metastatic lymph node involvement (New England Journal of Medicine, 2016). These therapies specifically target molecules that inhibit immune cells from recognizing and attacking cancer cells.
-
For cancers with specific genetic mutations (e.g., HER2-positive breast cancer), targeted drugs like trastuzumab have been shown to reduce the size of metastatic lymph nodes and improve survival (Lancet, 2002).
4. Prognosis and Follow-Up
Prognosis can vary depending on the number and size of metastatic nodes. Large nodes (typically those > 2 cm in size) are associated with worse prognosis, particularly if there are multiple nodes involved. Studies such as one in the Journal of Clinical Oncology (2006) have shown that the size and number of affected lymph nodes are independent predictors of survival in several cancers, including head and neck cancers and breast cancer.